Guide to BLS and ACLS Protocols for Emergency Care
Apr 13, 2023
Navigate Quickly
BLS Protocol
Pediatric Age Group Guidelines
ACLS Protocol
CPR Quality
Defibrillation
Airways

ACLS and BLS are life support measures employed by medical practitioners. BLS means Basic Life Support and employs measures that are performed in the basic stages of an emergency. On the other hand, ACLS translates into Advanced Cardiovascular Life Support. ACLS protocol includes supportive medical care that healthcare professionals need to perform in the hospital.
ACLS and BLS protocols are crucial topics for Medicine paper. Read this topic thoroughly to master ACLS and BLS protocols and ace your NEET PG preparation.
- BLS/ACLS protocols help us save precious lives. BLS stands for Basic Life Support. ACLS stands for Advanced Cardiac Life Support. Any person can provide BLS, but medical professionals can provide only ACLS. No drugs are needed to be given in BLS. In ACLS, medications are required, which a non-specialist cannot administer. Any person can provide basic life support to a patient until an emergency team arrives and save a precious life.
.jpeg )
BLS Protocol
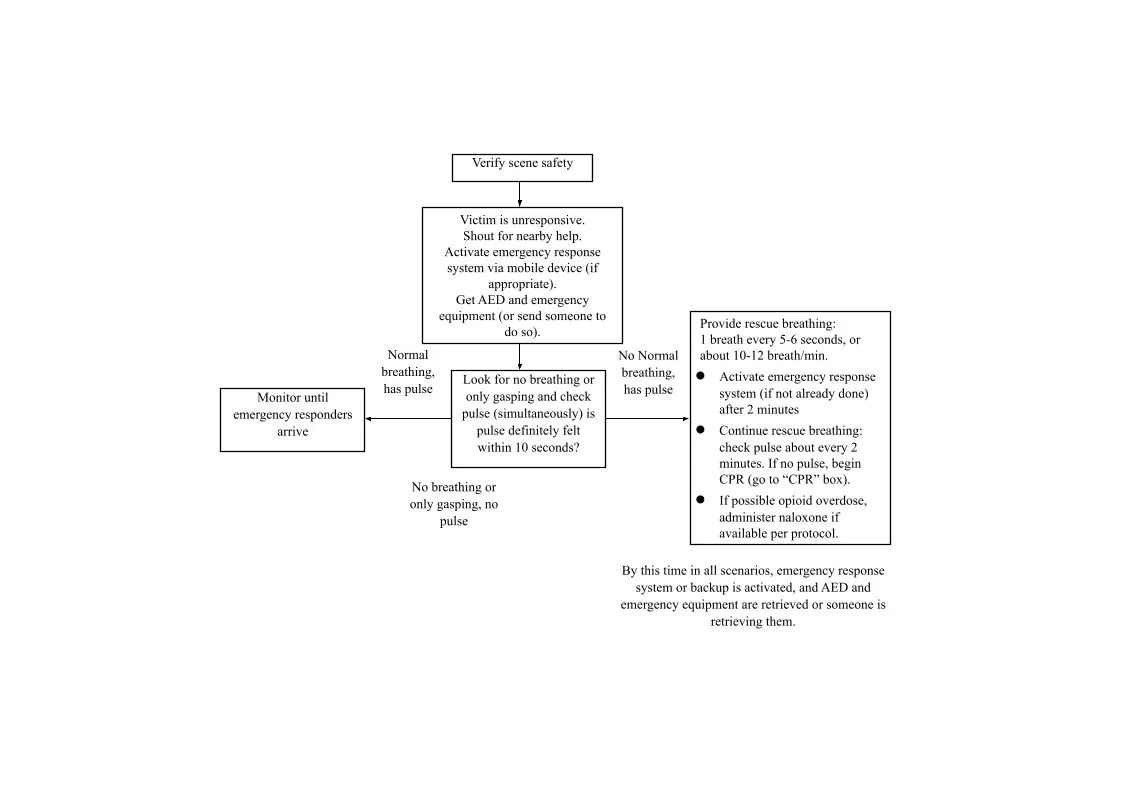
- American Health Association provides all the guidelines mentioned in the protocol. Verify scene safety: When a patient is found lying on the ground, see whether the site is safe. If not, look for a safe place. For example, if a patient is found unconscious on the road, instead of starting maneuvers right there, shift the patient to the roadside. If the patient is unresponsive, shout for nearby help, activate the emergency response system to call for an ambulance, etc. Get AED (Automated External Device) and medical equipment, or send someone else to do so. Most public places have AEDs, like malls, highways, petrol pumps, etc.
- See whether the patient is breathing or not. There can be three scenarios in this situation:
- The patient has normal breathing with a pulse: In this case, monitor the patient until emergency responders arrive. The patient is not breathing properly but has a pulse: In this case, CPR is not needed because the patient has a pulse. Instead, provide rescue breathing to the patient. Support the patient's breathing by giving 1 breath every 5 to 6 seconds or 10 to 12 breaths per minute. Continue rescue breathing and check pulse after every two minutes. Neither the patient is breathing properly nor has a pulse: If the patient loses their pulse, initiate CPR (Cardiopulmonary resuscitation). Start with chest compressions. Give 30 compressions and two breaths. Use AED as soon as it arrives.

- AED has two patches that get attached to the sternum and apex of the heart. It allows for checking the rhythm of the patient’s heart. It is well-made equipment. Only the instructions need to be followed when using it. AED tells whether the rhythm is shockable or not. There are four types of rhythms:
- Ventricular Tachycardia
- Ventricular Fibrillation
- Asystole
- Pulseless Electrical Activity
- Only ventricular tachycardia and ventricular fibrillation are shockable rhythms. If the machine detects that the rhythm is shockable, it delivers the shock and commands the user to resume CPR for two minutes. Resume CPR for two minutes after every shock. After some time, there will be a blink on the machine to check whether the patient has got his rhythm back or not. Keep on doing this until ALS providers take over the victim and start doing maneuvers like endotracheal intubation, administration of drugs, or shifts to the ambulance. If the rhythm is non-shockable, the machine will not deliver a shock. It will prompt you to resume CPR for two minutes. After that, the machine will automatically tell whether the rhythm is normal. A shock is not given in asystole and pulseless electrical activity. No medications are given in BLS protocol.
Pediatric Age Group Guidelines
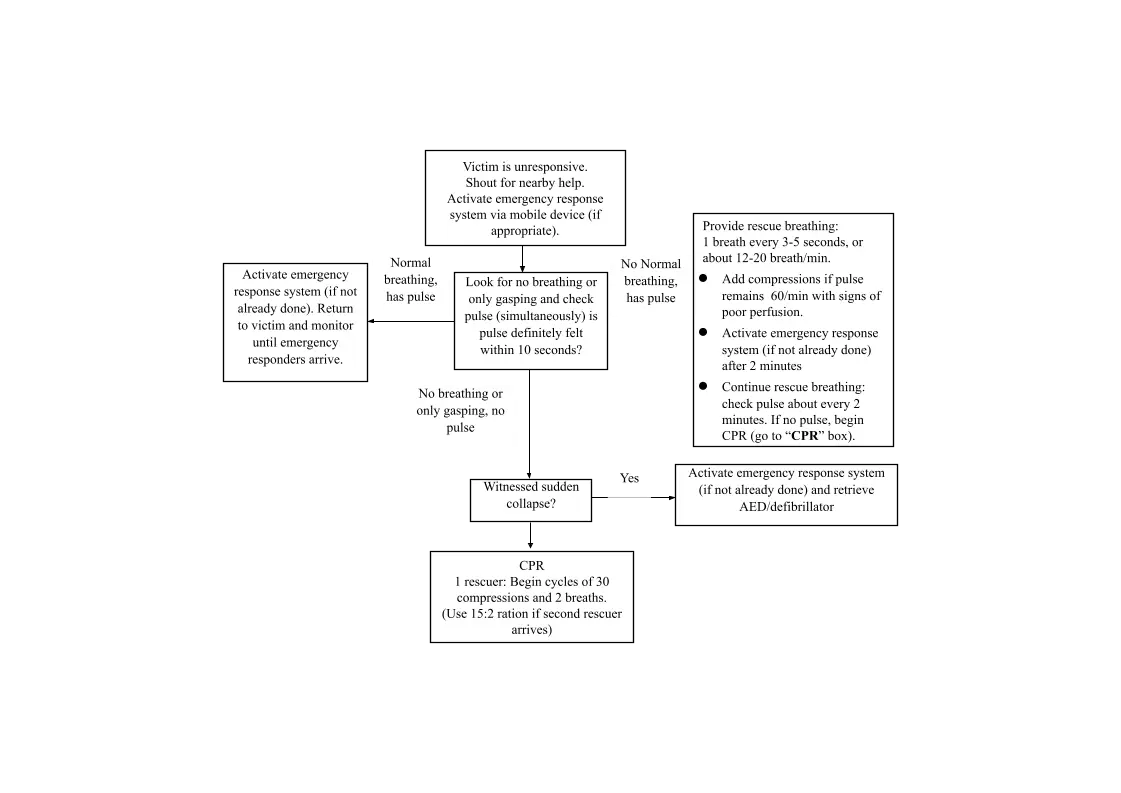
- The BLS guidelines for the pediatric age group vary depending on the number of rescuers. There can be a single rescuer or multiple rescuers. In the case of a single rescuer, verification of scene safety is a must here as well. Next is shouting for help and activation of the emergency response system. The oxygen requirement is more in the case of pediatric patients. So, whether the patient is receiving a proper oxygen supply needs to be checked, as well as their heart rate. If the patient has no normal breathing but has a pulse, 1 breath every 3 to 5 seconds is given (or about 12-20 breaths a minute) because the pediatric age group has a higher respiratory rate than adults. If the pulse rate remains less than 60/min with signs of poor perfusion, add compressions.

- For one rescuer, begin cycles of 30 compressions and two breaths. If the second rescuer arrives, use a 15: 2 ratio. It means 15 compressions and 2 breaths. This method has a better outcome for pediatric patients. If there are two or more rescuers, the pediatric algorithm remains the same. If there’s a single rescue, 30:2 is the compression-to-ventilation ratio. If the second rescuer arrives, use a 15: 2 ratio.
| Infant | Paediatrics |
| C:V = 30:2 | C:V = 30:2 |
| C:V = 15:2 | C:V = 15:2 |
| Pulse – Brachial Pulse | Carotid or Femoral Pulse |
- There’s a difference in guidelines between infants and pediatric age groups. The only difference is that brachial pulse is checked in infants to check whether there’s a return of circulation. In pediatric patients and adults, the carotid or femoral pulse is checked.
ACLS Protocol
- After the initial treatment, an ambulance arrives. The technical team consisting of doctors, nurses, etc., starts to do maneuvers on the patient. The CPR is continued, as before. Now, oxygen is given to the patient via an external device. A defibrillator is attached to check whether the rhythm is shockable. If a defibrillator delivers a shock, ventricular tachycardia or fibrillation is the rhythm. If it does not give any shock, the rhythm is asystole or PEA. The CPR is continued if the rhythm is shockable. In the meantime, Intravenous and Intraosseous access is secured. Again, see whether the rhythm is shockable or not. If it is shockable, the patient is administered epinephrine after the delivery of the second shock. If the patient is not revived, CPR is to be continued. Epinephrine is given every 3 to 5 minutes. Advanced airways (securing an endotracheal airway) are considered after delivering the second shock. It’s done to avoid any kind of aspiration in the patient. Capnography of the patient is seen afterward to check whether CPR is effective or not). If the rhythm is shockable again, a third shock is delivered. Amiodarone or lidocaine are given after the shock.
- There are ten different types of reversible causes that may cause cardiac arrest in the patient (5 Hs and 5Ts).
- Hypovolemia
- Hypoxia
- Hydrogen ion (Acidosis)
- Hypo-hyperkalemia
- Hypothermia
- Tension pneumothorax
- Tamponade cardiac
- Pulmonary thrombosis
- Coronary thrombosis
- Toxins
- In case the patient only has asystole or PES, then there is no need to deliver any shock. CPR and epinephrine are the only two options. After every two minutes, it’s checked whether the rhythm is shockable or not. Once shockable, the protocol of shockable rhythms is followed. The capnography graph above indicates the return of spontaneous circulation. If the patient’s end-tidal Co2 was around 10 before revival and came out to be 30 afterward, it means the patient has been revived and can be shifted to the hospital for further treatment. If it reaches 5 or even 0, the patient is dead.
CPR Quality
- Push hard (at least 5 cm (2 inches) and fast (100-120/min) and allow complete chest recoil. Minimize interruptions in compressions. Avoid excessive ventilation. Change compress or every 2 minutes, or sooner if fatigued. If no advanced airway, 30:2 compression-ventilation ration. Quantitative waveform capnography
- Petco 2 < 10 mm Hg, attempt to improve CPR quality.
- Intra-arterial pressure
- If relaxation phase (diastolic) pressure < 20 mm Hg. Attempt to improve CPR quality
- For good quality CPR, a person has to push hard and fast (at least 5 cm and 100-120 times a minute). The chest should be allowed to recoil properly. There should be minimal interruptions in chest compressions. If tired, the compressor has to be changed every two minutes for the best results. If there’s no advanced airway, the compression: ventilation ratio should be 30:2. Capnography shows CPR quality. If capnography shows below 10 mm, CPR quality needs to be improve
Defibrillation
Shock Energy for Defibrillation
- Biphasic: Manufacturer recommendation (eg. Initial dose of 120-200 J): If unknown, use maximum available. Second and subsequent doses should be equivalent and higher doses may be considered. Monophasic: 360 J
- There are two types of defibrillators: - biphasic and monophasic.
- Biphasic come in a range of 120-200 Joules. Monophasic comes in a range of 360 Joules. Irrespective of the type, maximum energy available must be used.
Drug Therapy
- Epinephrine IV/10 dose:
1 mg every 3-5 minutes
- Amiodarone IV/10 dose: First dose: 300 mg bolus, Second dose: 150 mg
Or
Lidocaine IV/10 dose:
First dose: 1-1.5 mg/kg.
Second dose: 0.5-0.75 mg/kg
- Drugs like epinephrine and amiodarone are given, but only in ACLS guidelines. Drugs are not used in BLS guidelines.
Airways
Advanced Airway
- Endotracheal intubation or supraglottic advanced airway . Waveform capnography or capnometry to confirm and monitor ET tube placement Once advanced airway in place, give 1 breath every 6 seconds (10 breaths/min) with continuous chest compressions. Endotracheal intubation or supraglottic advanced airways are used to secure airway of the patient. Waveform capnography or capnometry is used to confirm and monitor ET tube placement. Once the advanced airway is in place, one breath every 6 seconds in the norm.
ROSC (Return of Spontaneous Circulation)
- Pulse and blood pressure. Abrupt sustained increase in PETCO2 (typically > 40 mm Hg) . Spontaneous arterial pressure waves with intra arterial monitoring . ROSC is the Return of Spontaneous Circulation . It means a patient’s pulse and blood pressure return to normal after CPR.
- There’s an abrupt increase in the end-tidal CO2. It can be seen in a capnograph. It makes capnography very helpful for a patient when giving CPR.
That is everything you need to know about BLS and ACLS protocols for your Medicine preparation. For more interesting and informative posts like this, download the PrepLadder App and keep following our blog!

PrepLadder Medical
Get access to all the essential resources required to ace your medical exam Preparation. Stay updated with the latest news and developments in the medical exam, improve your Medical Exam preparation, and turn your dreams into a reality!
Top searching words
The most popular search terms used by aspirants
- NEET PG Medicine
PrepLadder Version X for NEET PG
Avail 24-Hr Free Trial