Neuroblastoma -Investigation, Staging and Treatment
Nov 17, 2023

Neuroblastoma -most common intra-abdominal tumor in children. Most common malignancy in the first year of life. It can occur in neonates and fetus. Most common extracranial solid tumor in children. 98% are sporadic, and 2% familial. 90% are vasoactive and produce catecholamine and its derivatives, such as VMA and HVA. The most common age group -0-5 years. The origin of cells for neuroblastoma are primitive neural crest cells.
Risk Factors Of Neuroblastoma
- Risk factors and associations of neuroblastoma are as follows. Neurofibromatosis-1, Hirschsprung disease, Heterochromia iridis, Fetal hydantoin syndrome, Fetal alcohol syndrome, Friedrich ataxia
Familial Neuroblastoma
- Most familial neuroblastomas have mutations in the ALK(anaplastic lymphoma kinase) gene, PHOX2B, and BARD1 genes. Deletion of chromosome 1p or rearrangement seen in 80% of cases. Associated with N-myc oncogene amplification in about 20% of cases and causes aggressive diseases.
.png)
Pathology Of Neuroblastoma
- Grossly, soft, rounded, heterogeneous masses that tan to pale grey with hemorrhage, cyst formation, punctate calcification, and necrosis. A fibrous pseudo-capsule may be seen.
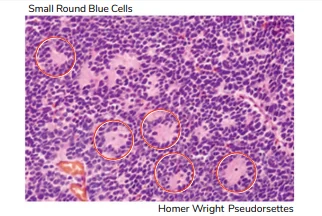
Histopathology Of Neuroblastoma
Histology - Solid sheets of small round blue cells. The cells may show mitotic activity, karyorrhexis, and pleomorphism. The background has faintly eosinophilic material composed of neuritic processes of primitive neuroblasts called neuropil. Homer-Wright pseudo rosettes- tumor cells arrange as a rosette with a neuropil in the center. Immunohistochemistry is positive for neuron-specific enolase. Electron microscopy shows cytoplasmic granules filled with catecholamine called dense core granules. Neuroblastoma showing hemorrhage, necrosis, and whitish calcification.

Also Read: KAWASAKI DISEASE : History, Symptoms, Causes and Treatment
Clinical Features Of Neuroblastoma
- Constitutional features: Low-grade fever, malaise, loss of appetite, weight loss, and night sweats. Abdominal mass-It is predominant in neuroblastomas arising from the adrenal medulla, painless. Features due to the release of vasoactive peptides. The release of catecholamines causes episodes or outbreaks of hypertension, excessive sweating, diarrhea (vasoactive intestinal peptide), and autonomic dysfunction.
- Features related to metastasis: The most common site of metastasis -bone, including the skull, long bones, and spine. The clinical features include. Bony pain and irritability, limping, Proptosis, Raccoon eyes, Vertebral collapse. The involvement of bone marrow causes cytopenia in the late stages. Due to associated syndrome or paraneoplastic syndrome.

Syndromes Associated With Neuroblastoma
|
Syndromes |
Features |
|
Pepper syndrome |
|
|
Horner syndrome |
|
|
Hutchinson disease |
|
|
Kerner-Morison syndrome |
|
|
Opsoclonus-myoclonus-ataxia syndrome Or Dancing eyes-dancing feet syndrome |
|
|
Neurocristopathy syndrome |
|
|
ROHHAD |
Approximately 40% have neural crest-derived tumors, including neuroblastoma. |
Q. Name the syndrome that increases Will’s tumor and neuroblastoma risk.
A. Beckwith-Weideman syndrome.
It poses a 30-75% risk of Will’s tumor and 5-10% neuroblastoma in children.
Q. What are the sites of metastasis of neuroblastoma?
A. Site of metastasis- lymph nodes, bones, bone marrow, and liver.
Pulmonary metastasis is rare in neuroblastoma.
Also Read: The Genetics of Down Syndrome
Investigations Of Neuroblastoma
- Gold standard tests - biopsy and immunohistochemistry. CT scan shows supra-renal calcification. MRI shows paraspinal tumors.- Iodine-123 or 131 MIBG and PET scan for the diagnosis of metastasis. About 95% of patients show elevated tumor markers, urinary VMA and HVA.
- Old staging of neuroblastoma according to the INSS classification system. Criteria for staging are as follows. Stage 1 – localized and completely resectable tumors. Stage 2 – incompletely resectable. Stage 3 – cross the midline. Stage 4 – disseminated or metastatic.
Staging Of Neuroblastoma
- The international neuroblastoma risk-group staging system recently revised the grading criteria as follows. L1 tumors (previously classified as INSS stage 1) are localized and confined to one body compartment without any Image Defined Risk Factors (IDRF). L2 tumors (previously classified as INSS stage 2 and 3) are localized tumors with the presence IDRF. M tumors are disseminated metastasized tumors to bones, bone marrow, liver, distant lymph nodes and other organs. (Previously classified as INSS stage 4). Stage MS (previously stage 4S) is neuroblastoma in children younger than 18 months and showing spontaneous regression.
Stage MS
- Stage MS is also called stage 4S. Mainly seen in age group <18 months. The earlier the age of incidence, the better the outcomes. The clinical features include-Widespread subcutaneous nodules, massive hepatic involvement, a small primary tumor, the involvement of bones and bone marrow is minimal, Show autoregression, excellent prognosis -survival rate >= 85%
Also Read: Pigmentary Disorders in Children
Treatment For Neuroblastoma
- Treatment is well-defined for each stage. Low-risk - include L1, L2, and MS, and their treatment s include. Primary surgery for L1. Surgery with or without chemotherapy for L2. Observation in most; chemotherapy for severely symptomatic stage MS patients
- Intermediate risk:- stages L2 and M with favorable prognostic factors- Surgery with chemotherapy, Radiotherapy in patients with aggressive and residual disease. The high-risk group - stage M cases with unfavorable prognostic factors. Palliative surgery has scope when the tumor is large. Chemotherapy with radiotherapy. Bone marrow transplantation. Isotretinoin or 13-cis-retinoic acid. Dinutuximab: Antiganglioside GD2 monoclonal antibody has been recenlty FDA approved.
Also Read: Progeria- Pathogenesis, Clinical Features and Treatment
Prognostic Factors Of Neuroblastoma
Factors Favorable Unfavorable Stage 1, 2A, 2B, and 4S 3 and 4 Age Below 18 months Above 18 months Schwannian stroma Present absent Gangliocytic differentiation Present Absent Mitotic karyorrhectic index (increased proliferation and death rate) <200 per 5000 cells > 200 per 5000 cells Ploidy Hyper ploidy Nearly diploid Loss or deletion of 1p Absent Present Loss or deletion of 11q Absent Present Loss or deletion of 14q Absent Present Gain of 17q Absent Present N-myc Not amplified Amplified Expression of TRKA Present Absent Expression of TRKB Absent Present Neuritogenic genes mutation (ATRX and PTPRD) Absent Present
If you are preparing for NEET-SS 2024 and ahead, check out SS ELITE Plan (Version 3.0) and what makes it the perfect study resource for your super speciality preparation.

PrepLadder Medical
Get access to all the essential resources required to ace your medical exam Preparation. Stay updated with the latest news and developments in the medical exam, improve your Medical Exam preparation, and turn your dreams into a reality!
Navigate Quickly
Risk Factors Of Neuroblastoma
Familial Neuroblastoma
Pathology Of Neuroblastoma
Histopathology Of Neuroblastoma
Clinical Features Of Neuroblastoma
Syndromes Associated With Neuroblastoma
Q. Name the syndrome that increases Will’s tumor and neuroblastoma risk.
Q. What are the sites of metastasis of neuroblastoma?
Investigations Of Neuroblastoma
Staging Of Neuroblastoma
Stage MS
Treatment For Neuroblastoma
Prognostic Factors Of Neuroblastoma
Top searching words
The most popular search terms used by aspirants
- NEET SS Pediatrics
- NEET SS Pediatrics Important Topics
PrepLadder 4.0 for NEET SS
Avail 24-Hr Free Trial